Hip & Knee Surgery
Hip and Knee Pain – Causes and Treatments
Hip and knee pain can be caused by deformity, injury or most commonly Osteoarthritis – a condition that involves joint cartilage progressively wearing away. This leads to bone friction, swelling, pain, stiffness and instability.
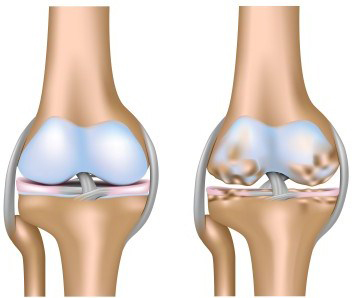
LEFT: Healthy Knee
RIGHT: Osteoarthritic Knee
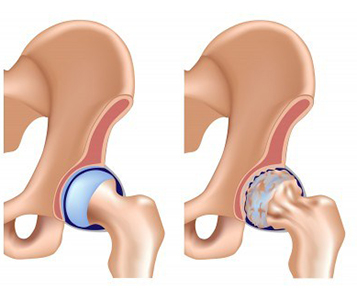
LEFT: Healthy Hip
RIGHT: Osteoarthritic Hip
If you are suffering from hip or knee pain, it is best to consult your GP who will discuss a range of treatment options with you. These could include weight management and exercise, rest and joint care, physiotherapy, or medication. Your GP might also refer you to an Orthopaedic specialist for further diagnosis and treatment.
Orthopaedic Surgery
Before any decisions are made, your orthopaedic surgeon will analyse your medical records closely, taking into consideration a letter from your regular doctor or rheumatologist, radiological and clinical exams, and your complete medical history. He or she might also perform an ‘Arthroscopy’ which involves inserting a small camera inside your hip or knee joint under anaesthetic to better diagnose problems. During this procedure, the surgeon might be able to repair tears in fibrous structures or torn ligaments, remove inflamed lining, or remove loose bone or cartilage.
If a further operation is considered necessary, your surgeon will describe the technical procedure best suited to your condition.
Hip Replacement Surgery
This involves replacing the head of the femur (the ball at the top of the thigh bone) and the acetabulum (hip socket).
Typically, the artificial ball and stem are made of a strong metal or ceramic, and the artificial socket is made of polyethylene liner (a durable, wear-resistant plastic) with a metal backed cup.
The artificial joint may be cemented in position or held securely in the bone without cement. The ball and insert are designed to glide together to replicate the hip joint.
Total hip replacement aims to providing long-term relief from pain, restore mobility, and improve quality of life for the patient.
Knee Replacement Surgery
During this procedure, your diseased or damaged joint is replaced with an artificial joint. It involves removing some small sections of bone where your femur (thigh bone), tibia (shin bone) and patella (kneecap) come together and replacing them with a combination of surgical-grade metal alloys and highly wear-resistant plastic.
The replacement joint is designed to move just like a healthy human joint and will help with pain and restore the bending and straightening movement of the knee.
The goal is to give you positive long term results by providing pain relief, restoring mobility, function and stability, and correcting deformity.
Your Surgery – What to Expect
BEFORE SURGERY
Medical Consultation and Informed Consent
You will consult with your orthopaedic surgeon and your anaesthetist who will explain the operating procedure and the possible risks and complications that could occur. These consultations are for you to raise any questions or concerns you may have.
The duty to inform the patient is a legal and ethical obligation required of the physician. All practitioners must inform the patient in order to obtain his/her consent for the care being proposed.
Your surgeon will also provide you with “post-surgery” information such as rehabilitation protocols, and the indications and limitations of use for your joint implant.
At the Hospital
Prior to admission remember to bring all your pre-operative results and radiological assessments (X-rays, MRI), health insurance information and the signed informed consent form. Also bring your toiletries and comfortable clothing for discharge from hospital.
Just before the procedure, your anaesthetist will visit you to finalise the last details of the operation. Finally, you and the anaesthetist will decide on the final care and monitoring strategy during and after the procedure and he/she will inform you about the procedure.
All jewellery, contact lenses, glasses, dentures and body piercing jewellery must be removed before you leave for the operating theatre.
If your wear dentures, please inform the surgical team and they will keep them safe for you.
You must have fasted prior to surgery following the physician’s instructions.
In the operating theatre
The operating theatre team will lead you to a pre-anaesthetic room where you will be briefed prior to the procedure. You will then be placed on the operating table in the operating room by the theatre nurses and the anaesthetist. Once all your vital functions have been verified, you will be anaesthetised according to the procedure chosen. Your procedure can then begin.
AFTER SURGERY
After your procedure, you will be monitored until you wake up in the recovery unit. A team of nurses will verify your vital signs (pulse, blood pressure, blood oxygen level) and assist you to reduce any pain you may be experiencing.
The days following surgery
Your surgeon will inform you how long you are likely to stay in hospital. Each surgery and patient result are unique. Your surgeon will also inform you if you are required to attend any specialist rehabilitation facility or follow a particular protocol.
The nurse will monitor your vital signs twice per day while you are in hospital. He/she will continue to evaluate pain and provide you with the suitable analgesic treatment. Your dressing will be checked daily.
Your physiotherapist will assist you for the duration of your hospitalisation. He/she will suggest exercises to enable you to regain your autonomy (walking, climbing stairs, etc.).
Your discharge is organised with your surgeon and healthcare team.
At Home
When retuning home it is important that you modify your home to facilitate your rehabilitation. This may include:
Avoiding stairs, which can be dangerous with crutches, so sleeping on the ground floor if your room is upstairs
- Using a raised toilet seat
- Having handrails installed in the shower and toilet
- Planning for an anti-slip bath mat and a shower stool with anti-slip legs (baths are not recommended at the beginning
- Wearing good bed slippers with anti-slip soles
- Being careful of slippery floors for the first few weeks: bathroom, kitchen, entrance
- Using high seats with armrest
Rehabilitation
Rehabilitation is very different from one person to the next; it depends on:
- Your age, needs, physical ability, vitality, and associated diseases
- The type of implant
- How the operation transpired and the outcome
- Your environment and your support system, family and friends
Your surgeon and physiotherapist/occupational therapist can guide you through any questions you may have and help to ensure that your home setup is adequate to facilitate your rehabilitation needs.
Possible Risks & Complications
While implants can greatly improve your mobility and lifestyle, they also have their limits. The following are some risk factors and complications you should be aware of.
EARLY COMPLICATIONS
Every surgical procedure involves risks; the presence of associated diseases can increase these risks. The main complications related to joint replacement surgery are the following (this list is not exhaustive):
Infection
This is a rare but serious complication that often requires a repeat procedure (to clean the operated joint and sometimes change the implant) and long-term antibiotic treatment. Infection can occur early after the procedure and in this case, is due to contamination of the operating site, usually by the skin.
Infection prevention measures are implemented by you prior to your surgery, during your hospital stay and post operatively.
An infection can occur later on, due to a germ transported by the blood. There are certain factors that contribute to infection: immunomodulatory treatment that weakens the body’s defence mechanisms (chemotherapy, disease-modifying drugs for rheumatoid arthritis, etc.), long-term use of corticosteroids, diabetes, and obesity. These factors will be discussed with you.
Blood effusion
There can be blood effusion in the joint (haemarthrosis) or the formation of a haematoma. This effusion might be minor and relieved by applying ice on the operated limb. If it is excessive, needle aspiration or even a surgical procedure, might be required to evacuate it.
This risk is prevented by careful vascular coagulation during the procedure, by the placement of drains when the surgical wound is being closed (to pull up and evacuate blood) and with the use of a compression bandage. This complication is rare in the hip and somewhat less rare in the knee.
On the contrary, ecchymosis (blue colouring of the skin) is common.
Dislocation
Dislocation of the implant is a complication that can occur during a high-risk movement or fall (especially during the first three months after the procedure), when the muscles surrounding the implant are too weak. This complication mostly applies to hip replacement implants. To prevent this complication, it is important to avoid certain movements as advised by your surgeon and physiotherapist, especially during the first three months after the operation.
Venous complications
Phlebitis (inflammation of a vein) can become venous thrombosis (clot in the vein). Immobilisation contributes to it. A fragment of the clot can sometimes detach and migrate to the lungs: this is a pulmonary embolism. The risk of thrombosis is now rare because of exercises to stimulate venous return in the legs, early mobilisation, anticoagulant treatment (that thins the blood) starting on the day before the procedure, and wearing support stockings.
Bone fracture
This can occur when the implant is being placed: this is also a very rare complication that is due to bone fragility. This complication can make placement of the implant somewhat more difficult.
Neuroparalysis
This is a very rare complication that affects the nerves located close to the implant, which can be harmed during the implantation procedure. Usually the paralysis regresses, but recovery can take several months.
LATER COMPLICATIONS
Wear
This invariably occurs for all implants and causes the implant to loosen. Loosening of the implant (loss of fixation of the components) manifests itself through pain and migration of the implant components; it can require a revision of the implant components.
Late infection
This occurs either via the blood from an infectious focus (skin, urine, bronchi, vesicle, sinus, etc.) or is due to a surgical contamination that went unnoticed, that develops silently and can lead to septic loosening of the implant.
Periprosthetic bone formation
This is rare. The bone that could form around the total hip replacement implant after the procedure could result in joint stiffening. This is prevented by the systematic use (except in the case of a specific contraindication) of non-steroidal anti-inflammatory drugs for a few days after the procedure. This complication mainly affects hip replacement implants.
Stiffness in a replacement joint
This can occur with certain implants, such as in the knee, elbow or shoulder. This is due to the presence of adhesions that limit mobility (the soft tissues are “stuck” together). It can be prevented by early gentle mobilisation of your implant, passive mobilisation or a manipulation under anasthetic.
Complex regional pain syndrome
This is a “deregulation of the nervous system that controls the vessels” and it causes pain, swelling and can result in stiffening of the joint. It is a complication that occurs and develops in an inconsistent and unpredictable way. Treatment is based on a combination of medicines and gentle specialised rehabilitation. The progression can be over several months.
Chronic effusion
There is swelling in the replacement joint, especially in the knee, which can require a puncture to verify the absence of infection. Specific local actions can be discussed and carried out in agreement with the surgeon in a specialised service, to dry out the effusion (isotopic synoviorthesis).
Venous thrombosis
This can occur long after the procedure: if you are experiencing pain in a calf, or are out of breath, please consult your physician.
If there is anything you are unsure about following your surgery, please speak to your doctor.
Customer Service and Logistics
E. customerservice@amplitude-ortho.com.au
T. 08 8297 9901
38 Payneham Road
Stepney, SA, 5069
Australia
Sales and Marketing
E. marketing@amplitude-ortho.com.au
Suite 6, The Village, 3 Julius Avenue
North Ryde, NSW, 2113
Australia